
Exploring Air Medical Transport in the U.S.
Chapter 5: COST AND ACCESS
Three Reasons Cost is a Challenge
While the air ambulance industry does a lot of good, cost is still a major factor that limits the accessibility of care. With rising prices, a lack of insurance for many patients, and deregulation of the industry, consumers are often faced with seemingly insurmountable bills.
1. Deregulation
In 1978, President Jimmy Carter signed the Airline Deregulation Act. Previous barriers were set forth by the Civil Aeronautics Board (CAB) which regulated where airlines could fly, and how much they could charge. With the introduction of this deregulation, the CAB was dissolved, and airlines could now set their own prices.
This also impacted air ambulance services, which could now operate as airlines and set prices as they saw fit. This left states unable to regulate these services or protect consumers from practices that took advantage of the new law.

2. Rising Prices
According to Research 360, a third-party organization that tracks the air ambulance industry, the average bill from Air Methods, the largest for-profit air medical transport operator, rose from $13,000 in 2007, to $50,000 in 2016.
The average bill for the industry as a whole was $30,895 in 2014.
But the real cost averages about $7,000, while New Mexico's Office of Superintendent of Insurance states that the average cost is about $10,000.

3. Lack of Insurance
For many patients, air ambulance coverage is considered "out of network" for providers. This means they are often not fully covered by insurance. According to an article by Consumer Reports, one family was left with a balance of $18,300 after their insurance company, Blue Cross and Blue Shield, paid only $5,700 of their $24,000 bill.
LifeFlight of Maine's Director of Development Amy Root said, "In an ideal world if you are a patient and you had tremendous health insurance, we would charge you and your insurance would cover the cost." But in actuality, LifeFlight of Maine diverts a tremendous amount of funds to charity care, in order to cover costs for patients who can't afford their transport bills.
But for other patients, support through charity care is not an option, and many are left with crippling debt, and bad credit.

POLITICAL IMPLICATIONS
In today’s tumultuous political climate, access and affordability of healthcare is a hot topic. However, these issues become even more problematic when looking at how access and affordability differs when race and ethnicity play a role.
Health and Healthcare Disparities
Health Disparity: "a higher burden of illness, injury, disability or mortality experienced by one population group relative to another."
Healthcare Disparity: "differences between groups in health insurance coverage, access to and use of care, and quality of care."
These issues are typically viewed through the lens of race and ethnicity, but they also affect a variety of other groups as well. Factors include age, geography, language, gender, socioeconomic status, and sexual orientation.
These disparities are not a new concept, and have been present in the United States for decades. They persist, and in some areas, are even widening.
Source: The Kaiser Family Foundation
Who is Impacted?
In general, people of color tend to face more of these barriers than Whites, and will often utilize less care. A study conducted by the Kaiser Family Foundation found that among older adults, people of color, including Hispanics, Blacks, American Indians, and Alaska Natives, were more likely than their White counterparts to delay or go without necessary care.
Low income families and individuals also experience these barriers, and tend to receive lesser quality care than those in high-income households. Sexual orientation also plays a role, and members of the LGBT community often face challenges when trying to obtain care.
Language and English proficiency may also determine who is more likely to seek care. Those who are English proficient tend to seek care, while those who may have limited English skills will go without, even when they are insured.
Some groups also experience higher rates of specific conditions, and their identity can reflect their health outcome. Blacks, American Indians, and Alaska Natives have higher rates of asthma, diabetes, and cardiovascular disease and tend to fare far worse than Whites when struggling with these conditions.
Source: Kaiser Family Foundation



Why Do These Disparities Matter?
Health and healthcare disparities affect many different people, but they also limit the ability to improve the quality of care for a broad population across the healthcare system.
The United States population is projected to become even more diverse over the course of the next few decades, and data shows that people of color will make up over half the population in 2045.
Income inequality is also on the rise, and large gaps continue to grow between the wealthiest, and poorest households in most states. In addition, the Kaiser Family Foundation notes that, "Given that people of color make up a disproportionate share of the low-income and the uninsured relative to their size in the population, the growth of communities of color and widening of income gaps amplify the importance of addressing health and health care disparities."
Air medical transport is an important and necessary facet of the healthcare system. However, certain groups who experience widespread disparities may not have access to these services, or may decide to delay necessary care.
In addition, certain areas of the U.S. are highly segregated, and New England tends to be predominantly white. While non-profit services may try to keep their prices lower, there is still a large gap between those that can afford this service, and those that cannot.
Source: Kaiser Family Foundation


Spotlight On: Fundraising Efforts at LifeFlight of Maine
High Operating Costs
LifeFlight of Maine is a non-profit organization that receives most of its day-to-day income from insurance payments and patient billing.
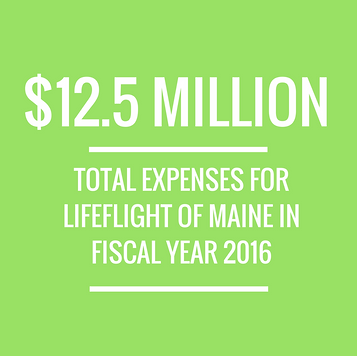
In 2016, the expenses for the organization totaled almost $12.5 million dollars. This amount includes funds for facility upkeep, medical equipment, aircraft replacement, administration, and dispatch communications. Expenses were even higher this past year when the organization added a third helicopter to its fleet.
Lower Transport Costs
LifeFlight of Maine strives to keep its costs as low as possible, which means sometimes extra funds are needed to fill the gaps.
The organization relies on a variety of fundraising efforts to stay afloat. One of the biggest fundraisers for LifeFlight of Maine is the Islesboro Crossing Swim. This 5K swim crosses the West Penobscot Bay from North Port on the mainland, to the remote island of Islesboro.
This three-mile swim, now in its sixth year, attracts visitors from around the state who flock to participate each August. The swim is designed to show the challenges of providing critical medical care to Maine's remote communities that are bound by water.

Where is Islesboro?
Islesboro is an island located off the coast of central Maine. It is primarily a summer destination, and is accessible only by ferry or boat. It is just southeast of Bar Harbor and Acadia National Park, and sits in the Gulf of Maine roughly 3 miles offshore from nearby Lincolnville.

Island of Islesboro

Where do the funds go?

